Ryan visit promotes pharmacy reform legislation

Officials and pharmacists gathered at Pine Plains Pharmacy on Monday, Feb. 17, to underscore the need for pharmacy benefit manager reform, an effort toward fairness in drug prices for local family-owned pharmacies. Left to right are Chris Drago, Dutchess County legislator, D-Stanfordville; U.S. Rep. Pat Ryan, D-N.Y., at podium; Pine Plains pharmacist Nasir Mahmood; area pharmacist Eric Lambert; Pine Plains pharmacist Rehan Mahmood; and Mark Freitas, Washingtonville pharmacist.
Photo submitted





















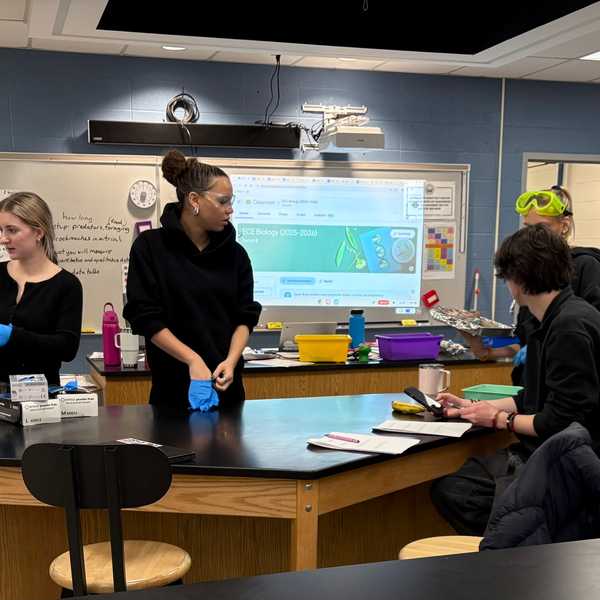
 Local parents, child care providers and nonprofit representatives outline the challenges they face in accessing and providing childcare in rural northeast Dutchess County during a forum at the Stissing Center in Pine Plains on Wednesday, Feb. 25. Photo by Nathan Miller
Local parents, child care providers and nonprofit representatives outline the challenges they face in accessing and providing childcare in rural northeast Dutchess County during a forum at the Stissing Center in Pine Plains on Wednesday, Feb. 25. Photo by Nathan Miller 


 lakevillejournal.com
lakevillejournal.com 



 Visitors consider Norman Rockwell’s paintings on Civil Rights for Look Magazine, “New Kids in the Neighborhood” (1967) and “The Problem We All Live With” (1963.) L. Tomaino
Visitors consider Norman Rockwell’s paintings on Civil Rights for Look Magazine, “New Kids in the Neighborhood” (1967) and “The Problem We All Live With” (1963.) L. Tomaino